- Compound Overview
- What is Retatrutide?
- What Does Retatrutide Do?
- Research Applications and Benefits of Retatrutide
- Side Effects of Retatrutide
- Is Retatrutide Safe?
- Is Retatrutide Legal?
- Retatrutide Dosing | Research Only
- Where to Buy Retatrutide Online? | 2024 Edition
- How to Reconstitute Retatrutide
- FAQ
- Retatrutide Review
- References
Compound Overview
Class of Compound:
Peptide
Mechanism of Action:
Retatrutide is a triple receptor agonist that targets the receptors of GIP, GLP-1, and glucagon hormones. By combining the effects of native GIP and GLP-1 with glucagon receptor activation, it exerts a broad appetite-suppressing and metabolic impact. Researchers suggest that this triple mechanism may offer more effective glycemic control and weight loss compared to other incretin-based therapies.
Notable Studies:
- Is retatrutide (LY3437943), a GLP-1, GIP, and glucagon receptor agonist a step forward in the treatment of diabetes and obesity?
- Retatrutide, a GIP, GLP-1 and glucagon receptor agonist, for people with type 2 diabetes: a randomised, double-blind, placebo and active-controlled, parallel-group, phase 2 trial conducted in the USA - The Lancet
- Triple–Hormone-Receptor Agonist Retatrutide for Obesity — A Phase 2 Trial | New England Journal of Medicine
Also Known As:
LY3437943
Research Applications:
- Weight loss,
- Glycemic control
- Improved metabolism
Risks:
- Gastrointestinal Issues
- Pancreatitis
- Hypersensitivity Reactions
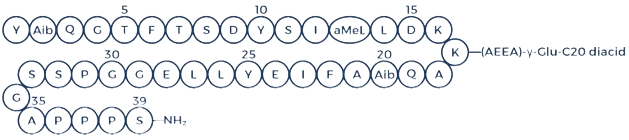
Chemical Structure
What is Retatrutide?
Retatrutide, a synthetic peptide created by Eli Lilly, is also known by its development code LY3437943. This peptide acts as a triple receptor agonist, targeting the glucagon-like peptide-1 (GLP-1), glucose-dependent insulinotropic polypeptide (GIP), and glucagon (GCG) receptors [1].
Both GLP-1 and GIP are incretin hormones that stimulate insulin secretion and modulate immune responses. Moreover, the activation of GCG receptors by retatrutide is thought to boost metabolic rate and increase energy expenditure [2].
This cutting-edge compound is being explored for its role in controlling blood glucose levels and aiding in weight loss [3].
Important details for researchers:
- Developed by Eli Lilly, retatrutide is a synthetic peptide based on the structure of GIP and is composed of 39 amino acids. While it predominantly targets GIP receptors, it has been engineered to also activate GLP-1 and GCG receptors [4].
- Retatrutide features a structural modification with a fatty acid component, which enhances its stability and prolongs its activity in the body, allowing for once-weekly dosing [5].
- Currently, retatrutide is undergoing evaluation in clinical trials for its safety and effectiveness in treating obesity, both in individuals with and without type 2 diabetes (T2D), as part of Eli Lilly’s TRIUMPH phase-3 clinical program [3].
- Initial study results have indicated positive outcomes for both glycemic control and weight loss [6, 7].
Although it has not yet been approved by regulatory authorities such as the U.S. Food and Drug Administration (FDA), retatrutide is available to qualified researchers as a reference material for studying the therapeutic potential of this triple receptor agonist.

What Does Retatrutide Do?
Retatrutide operates through a unique mechanism as a triple agonist, targeting the GIP, GLP-1, and GCG receptors, with a strong emphasis on GIP receptor activation [4].
Incretin hormones GLP-1 and GIP stimulate insulin secretion from pancreatic beta cells and contribute to feelings of fullness after eating, while glucagon serves a counter-regulatory function by raising blood glucose levels during fasting.
This receptor interaction leads to a comprehensive approach to metabolic regulation, significantly impacting both glycemic control and weight loss. Below is an overview of the underlying mechanisms:
- Retatrutide’s primary mechanism involves potent activation of the GIP receptor, which plays a vital role in appetite regulation by directly affecting the brain’s satiety centers. This reduces hunger, cravings, and overall food intake [8].
- Through GLP-1 receptor activation, retatrutide supports glycemic regulation and enhances satiety. GLP-1 also slows down gastrointestinal motility and delays gastric emptying, leading to increased feelings of fullness after meals [9, 10].
- Activation of the GCG receptor by retatrutide is believed to increase energy expenditure and promote fat oxidation, largely through metabolic actions in the liver. GCG receptor stimulation encourages fat breakdown and elevates metabolic rates. Additionally, it induces “beiging” of white fat, converting it into beige fat with thermogenic properties similar to brown fat, thereby boosting calorie burning and enhancing metabolism [11].
These combined mechanisms make retatrutide a promising option for treating obesity and type 2 diabetes by not only curbing calorie intake but also increasing energy expenditure, offering a dual strategy for effective weight management.
Research Applications and Benefits of Retatrutide
Outlined below you can find several key clinical trials that have demonstrated the efficacy and potential research applications of retatrutide.
Retatrutide and Weight Loss Research
As of 2024, phase 3 trials within the TRIUMPH program are in progress, exploring retatrutide’s potential for weight loss. Earlier phase 1 and phase 2 studies have shown promising results, indicating that the peptide could lead to up to a 24% reduction in body weight from baseline.
The initial human trial of retatrutide, a proof-of-concept study, took place in Singapore in 2019. This phase 1 trial involved 47 participants who were administered six different dose levels, ranging from 0.1 mg to 6 mg weekly. The study suggested potential positive effects on appetite, food intake, and other metabolic markers, alongside a favorable safety profile [4].
Following this, a larger phase 2 trial was conducted, lasting 48 weeks and involving 338 non-diabetic adults with overweight and obesity. Participants received varying doses of retatrutide, and the trial demonstrated a dose-dependent reduction in weight and improvement in cardiometabolic risk factors. Key findings included [7]:
- An 8.7% weight reduction in the 1 mg dose group
- A 17.1% weight reduction in the 4 mg group
- A 22.8% reduction in the 8 mg group
- A 24.2% reduction in the 12 mg group
All participants who received either 8 mg or 12 mg of retatrutide weekly experienced at least a 5% reduction in their initial body weight. In addition, significant reductions were observed in waist circumference, blood pressure, glycated hemoglobin, fasting glucose, insulin levels, and lipid levels, excluding HDL cholesterol.
Retatrutide and Type 2 Diabetes Research
Eli Lilly is conducting ongoing research on retatrutide’s potential to manage glycemic control and obesity in individuals with type 2 diabetes (T2D) as part of the phase 3 TRIUMPH clinical trials.
Earlier trials, including phase 1b and phase 2 studies, have shown encouraging outcomes. In a 12-week phase 1b trial, 72 adults aged 20-70 with T2D and baseline A1c levels between 7.0% and 10.5% were treated with either retatrutide, dulaglutide (a GLP-1 agonist approved by the FDA), or placebo.
By week 12, those receiving the highest dose of retatrutide (12 mg weekly) saw a significant decrease in A1c of up to 1.6% and a weight reduction of up to 19.7 pounds (8.96 kg). These results were markedly better than those seen with both dulaglutide and placebo [12].
A subsequent 36-week phase 2 trial involved 281 T2D patients receiving up to 12 mg of retatrutide weekly. Key results include [6]:
- Participants in the 12 mg group experienced a significant HbA1c reduction of 2.02% (22.07 mmol/mol) at 24 weeks and 2.16% (23.59 mmol/mol) at 36 weeks, compared to negligible change (0.01%) in the placebo group after 24 weeks.
- By the conclusion of the 36-week trial, weight loss was dose-dependent, with the 12 mg group losing 16.94% of their body weight, compared to a 3.00% reduction in the placebo group.
- Additionally, retatrutide treatment led to improved lipid profiles, including decreases in triglycerides and non-HDL cholesterol, with the 12 mg group showing significant improvement at 36 weeks compared to both baseline and placebo.
Buy Retatrutide from our top-rated vendor...

Side Effects of Retatrutide
Data from phase 2 trials indicate that retatrutide’s side effects are similar in severity and frequency to those associated with other GLP-1/GIP peptide analogs [6, 7].
In one of the phase 2 studies involving 338 non-diabetic participants, gastrointestinal disturbances were the most frequently reported side effects [7].
Here are the most common adverse events experienced by the 62 participants who received the maximum dose of 12 mg of retatrutide weekly:
- Pancreatitis: 2% (1 participant)
- Hepatic disorder: 3% (2 participants)
- Increased lipase levels: 8%
- Fatigue and early satiety: 10% each
- Cardiac arrhythmia: 11%
- Diarrhea: 15%
- Constipation: 16%
- Vomiting: 19%
- Nausea: 45%
Serious adverse events were similarly low between the retatrutide and placebo groups, with both at 4%. Among those taking retatrutide, 1% experienced temporary increases in alanine aminotransferase (ALT) levels exceeding three times the normal upper limit.
Additionally, increases in amylase and lipase levels were noted, though these were mostly asymptomatic except for one case of acute pancreatitis in the highest dose group.
Gastrointestinal issues were the leading cause of treatment discontinuation. In the treatment group, dropout rates due to adverse effects ranged from 6% to 16%, depending on the dose of retatrutide administered. There were no treatment-related dropouts in the placebo group [7].
Is Retatrutide Safe?
Retatrutide has not yet been approved for any form of human use; however, it is available to qualified researchers for studying its therapeutic potential as a triple receptor agonist.
Retatrutide is currently undergoing clinical development within Eli Lilly’s TRIUMPH phase-3 clinical program, which aims to gather extensive data on its efficacy and safety. This program is designed to provide comprehensive insights that could eventually support regulatory approval for medical use.
However, data from phase 1 and phase 2 trials suggest that the peptide is generally well-tolerated, with side effects similar to those observed with FDA-approved incretin mimetics such as dulaglutide, indicating a comparable safety profile.
Nevertheless, researchers using retatrutide in laboratory settings must remain mindful of potential risks, ensuring that all handling and experimentation are conducted under strict professional supervision.
Is Retatrutide Legal?
Retatrutide is not currently available as a prescription medication and has not been approved for human use in the United States or internationally. As of this writing, it remains under investigation in clinical trials for potential applications in treating conditions like type 2 diabetes and obesity, similar to other incretin mimetics.
Qualified researchers and laboratory professionals can legally obtain retatrutide as a reference material for research purposes. However, it is important to note that retatrutide is not available over-the-counter and cannot be used as a dietary supplement.
Unqualified use of retatrutide could lead to legal repercussions, and improper administration carries significant health risks. Researchers should avoid purchasing retatrutide marketed as a supplement or included as an ingredient in supplements, as such products are often of low quality and may pose serious dangers to research subjects.
Retatrutide Dosing | Research Only
Researchers are advised to follow specific dosing protocols to ensure the safety and efficacy of retatrutide in weight loss studies. The dosing regimen starts with a low dose of 1 mg per week, which is gradually increased to minimize side effects. The recommended schedule is as follows:
- Weeks 1-4: Start with 1 mg weekly
- Weeks 5-8: Increase to 2 mg weekly
- Weeks 9-12: Increase to 4 mg weekly
- Weeks 13-16: Increase to 8 mg weekly
- Week 17+: Reach the full dose of 12 mg weekly
It’s essential that researchers do not exceed the maximum recommended dosage of 12 mg per week. Retatrutide is designed for once-weekly subcutaneous administration, and due to its extended half-life, it can be injected at any time of day, with or without food [6, 7].
In clinical trials, the preferred injection site has been the abdomen, specifically at least 2 inches (5 cm) away from the belly button, to minimize the risk of bruising, redness, infection, or irritation. Studies have shown that retatrutide can be safely administered over a 48-week period, with a safety profile comparable to that of a placebo and other incretin mimetics [6, 7].
This long-term dosing approach indicates that retatrutide does not require cycling on and off, and sustained use is crucial for maximizing its therapeutic effects in weight management and metabolic health improvement.
Where to Buy Retatrutide Online? | 2024 Edition
Researchers looking to buy Retatrutide have several options available from various online vendors. However, it’s important to note that not all suppliers can be relied upon for quality.
For the best results, it’s crucial to obtain Retatrutide from thoroughly vetted sources. Our peptide review team has rigorously tested several suppliers, and the following consistently excel in peptide purity, timely delivery, and customer service:
Polaris Peptides
Polaris Peptides is an emerging supplier specializing in high-quality peptides intended solely for research and development by professionals. This vendor offers several key advantages:
- Purity and Accuracy: Polaris retatrutide is produced with meticulous precision, ensuring a purity level of over 99%.
- Transparency: Detailed lab results accompany every Polaris peptide for sale, providing you with the assurance of retatrutide’s quality and integrity.
- Customer Support: Polaris Peptides provides exceptional customer service, offering personalized assistance and fast shipping for a smooth purchasing process.
Buy Retatrutide from our top-rated vendor...

How to Reconstitute Retatrutide
Retatrutide is supplied as a lyophilized powder intended for research purposes and must be reconstituted with either bacteriostatic water or sterile water.
Bacteriostatic water, which contains 0.9% benzyl alcohol, is preferred for reconstitution because it inhibits bacterial growth, allowing the peptide to remain stable for up to four weeks when refrigerated properly at 36 to 46 degrees F (2 to 8 degrees C) [13].
In contrast, when sterile water is used, the peptide's stability lasts only 24 hours.
Researchers typically follow these steps for the reconstitution process:
- Assemble all necessary materials and let the retatrutide and bacteriostatic water vials come to room temperature, avoiding exposure to heat or sunlight.
- Clean the rubber stoppers of the vials with alcohol swabs to prevent contamination.
- Use a sterile syringe to draw air and inject it into the bacteriostatic water vial to facilitate the withdrawal of the liquid.
- Withdraw the required amount of water and carefully inject it into the retatrutide vial, directing the stream along the vial’s side to prevent foam formation.
- If sonication equipment is available, use it to speed up the dissolution of the powder; otherwise, allow the powder to dissolve slowly without shaking.
- Check the solution for clarity, and discard it if any turbidity or particles are present.
Following this protocol ensures proper reconstitution of retatrutide for research while maintaining accuracy and professionalism.
FAQ
Retatrutide Review
Although still in the development stage, retatrutide shows significant potential for various research applications. Currently undergoing phase 3 clinical trials, it is being evaluated for its effectiveness in managing type 2 diabetes and promoting long-term weight control.
Early studies suggest that retatrutide may offer benefits such as improved blood sugar regulation, appetite suppression, and fat loss. Additionally, researchers are exploring its possible cardiovascular advantages, which could enhance its value as a research tool.
Researchers interested in studying retatrutide for weight loss and other uses are encouraged to obtain the peptide in research-grade form from our most trusted supplier.

References
- Jakubowska, A., Roux, C. W. L., & Viljoen, A. (2024). The Road towards Triple Agonists: Glucagon-Like Peptide 1, Glucose-Dependent Insulinotropic Polypeptide and Glucagon Receptor - An Update. Endocrinology and metabolism (Seoul, Korea), 39(1), 12–22.
- https://doi.org/10.3803/EnM.2024.1942
Folli, F., Finzi, G., Manfrini, R., Galli, A., Casiraghi, F., Centofanti, L., Berra, C., Fiorina, P., Davalli, A., La Rosa, S., Perego, C., & Higgins, P. B. (2023). Mechanisms of action of incretin receptor based dual- and tri-agonists in pancreatic islets. American journal of physiology. Endocrinology and metabolism, 325(5), E595–E609. https://doi.org/10.1152/ajpendo.00236.2023 - Naeem, M., Imran, L., & Banatwala, U. E. S. S. (2024). Unleashing the power of retatrutide: A possible triumph over obesity and overweight: A correspondence. Health science reports, 7(2), e1864. https://doi.org/10.1002/hsr2.1864
- Coskun, T., Urva, S., Roell, W. C., Qu, H., Loghin, C., Moyers, J. S., O'Farrell, L. S., Briere, D. A., Sloop, K. W., Thomas, M. K., Pirro, V., Wainscott, D. B., Willard, F. S., Abernathy, M., Morford, L., Du, Y., Benson, C., Gimeno, R. E., Haupt, A., & Milicevic, Z. (2022).
LY3437943, a novel triple glucagon, GIP, and GLP-1 receptor agonist for glycemic control and weight loss: From discovery to clinical proof of concept. Cell metabolism, 34(9), 1234–1247.e9. https://doi.org/10.1016/j.cmet.2022.07.013 - Doggrell S. A. (2023). Is retatrutide (LY3437943), a GLP-1, GIP, and glucagon receptor agonist a step forward in the treatment of diabetes and obesity?. Expert opinion on investigational drugs, 32(5), 355–359. https://doi.org/10.1080/13543784.2023.2206560
- Rosenstock, J., Frias, J., Jastreboff, A. M., Du, Y., Lou, J., Gurbuz, S., Thomas, M. K., Hartman, M. L., Haupt, A., Milicevic, Z., & Coskun, T. (2023). Retatrutide, a GIP, GLP-1 and glucagon receptor agonist, for people with type 2 diabetes: a randomised, double-blind, placebo and active-controlled, parallel-group, phase 2 trial conducted in the USA. Lancet (London, England), 402(10401), 529–544. https://doi.org/10.1016/S0140-6736(23)01053-X
- Jastreboff, A. M., Kaplan, L. M., Frías, J. P., Wu, Q., Du, Y., Gurbuz, S., Coskun, T., Haupt, A., Milicevic, Z., Hartman, M. L., & Retatrutide Phase 2 Obesity Trial Investigators (2023). Triple-Hormone-Receptor Agonist Retatrutide for Obesity - A Phase 2 Trial. The New England journal of medicine, 389(6), 514–526. https://doi.org/10.1056/NEJMoa2301972
- Samms, R. J., Sloop, K. W., Gribble, F. M., Reimann, F., & Adriaenssens, A. E. (2021). GIPR Function in the Central Nervous System: Implications and Novel Perspectives for GIP-Based Therapies in Treating Metabolic Disorders. Diabetes, 70(9), 1938–1944. https://doi.org/10.2337/dbi21-0002
- Baggio, L. L., & Drucker, D. J. (2014). Glucagon-like peptide-1 receptors in the brain: controlling food intake and body weight. The Journal of clinical investigation, 124(10), 4223–4226. https://doi.org/10.1172/JCI78371
- Marathe, C. S., Rayner, C. K., Jones, K. L., & Horowitz, M. (2011). Effects of GLP-1 and incretin-based therapies on gastrointestinal motor function. Experimental diabetes research, 2011, 279530. https://doi.org/10.1155/2011/279530
- Conceição-Furber, E., Coskun, T., Sloop, K. W., & Samms, R. J. (2022). Is Glucagon Receptor Activation the Thermogenic Solution for Treating Obesity?. Frontiers in endocrinology, 13, 868037. https://doi.org/10.3389/fendo.2022.868037
- Urva, S., Coskun, T., Loh, M. T., Du, Y., Thomas, M. K., Gurbuz, S., Haupt, A., Benson, C. T., Hernandez-Illas, M., D'Alessio, D. A., & Milicevic, Z. (2022). LY3437943, a novel triple GIP, GLP-1, and glucagon receptor agonist in people with type 2 diabetes: a phase 1b, multicentre, double-blind, placebo-controlled, randomised, multiple-ascending dose trial. Lancet (London, England), 400(10366), 1869–1881. https://doi.org/10.1016/S0140-6736(22)02033-5
- Novak, E., Stubbs, S. S., Sanborn, E. C., & Eustice, R. M. (1972). The tolerance and safety of intravenously administered benzyl alcohol in methylprednisolone sodium succinate formulations in normal human subjects. Toxicology and applied pharmacology, 23(1), 54–61. https://doi.org/10.1016/0041-008x(72)90203-7
- Abbasi J. (2023). FDA Green-Lights Tirzepatide, Marketed as Zepbound, for Chronic Weight Management. JAMA, 330(22), 2143–2144. https://doi.org/10.1001/jama.2023.24539
- Melson, E., Ashraf, U., Papamargaritis, D., & Davies, M. J. (2024). What is the pipeline for future medications for obesity?. International journal of obesity (2005), 10.1038/s41366-024-01473-y. Advance online publication. https://doi.org/10.1038/s41366-024-01473-y
